How to avoid claim denials for crowns
Have you received denials for your claims for crowns? There may be many reasons ranging from incorrect documentation to the condition of the tooth or gums. Here’s a look at the documentation and processing guidelines for submitting claims and pre-authorizations for crowns (D2710–D2794).
Before submitting a claim for a crown, make sure you’ve met the requirements needed to ensure coverage for the procedure. Ask yourself these questions to confirm your claim meets Delta Dental policies.
Do you have appropriate pre-operative periapical radiographs?
To submit claims for a crown, you’ll need a pre-operative periapical radiograph showing the state of the tooth. It needs to have been taken within one year of the crown prep procedure. Be sure to include periapical radiographic images showing both the apex and clinical crown, because the teeth must be evaluated for periapical pathosis. Don’t substitute a panoramic radiograph to replace these periapical images.
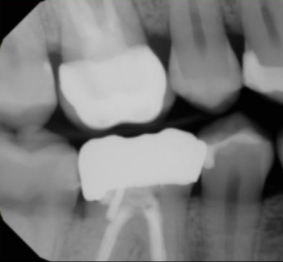
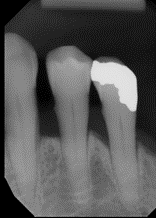
In the following example, the claim was submitted for a crown on tooth #30. However, the radiographic image doesn’t show the tip of the tooth’s roots. Pre-operative radiographic images must show the apex.
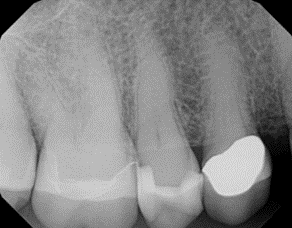
In comparison, the following pre-operative radiographic image correctly shows the apex of tooth #4.
Top crown denial codes due to inadequate x-rays
The codes most often associated with crown denials due to x-ray requirements include:
- 5RX. The submitted radiograph doesn’t show the entire tooth.
- 570 and SL8. Pre-operative periapical radiographic images are missing.
- 569. The radiographic images submitted aren’t diagnostic.
Have I met the crown requirements for an anterior or posterior tooth?
To qualify for full crown coverage on an anterior tooth, at least one of the following criteria must apply:
- The tooth must demonstrate at least 50% loss of structure and affect one or both incisal angles. For cuspids, the tip of the cusp must be affected.
- Existing restorations need to be replaced due to caries, fractures or missing tooth structure.
- At least half of the incisal angle needs replacing due to decay or fracture.
- There must be large existing restorations involving both mesial and distal surfaces, encompassing at least half of the tooth structure that requires replacement due to decay or fracture.
To qualify for full crown coverage on a posterior tooth, at least one of the following criteria must apply:
- The tooth has significant missing structure (greater than 50%) including loss of or undermining of one or more cusps and a compromised mesial or distal marginal ridge.
- There must be a large area of decay on a previously unrestored surface.
- There is extensive recurrent decay.
- The tooth must be endodontically treated.
- There is evidence of a cuspal fracture.
In cases where crowns may not appear to meet criteria for full crown coverage, pre-operative intra-oral photographs may also be submitted as supporting documentation in addition to radiographs.
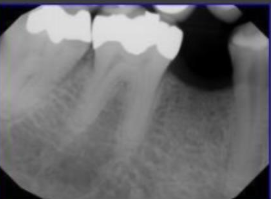
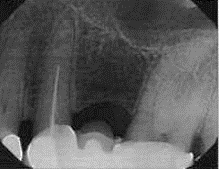
In the following example, the claim was submitted for a crown on tooth #3. However, the pre-operative radiographic image doesn’t show an extensive loss of tooth structure due to decay, existing large restorations or fracture. The existing occlusal restoration is shallow with minimal recurrent or interproximal decay.

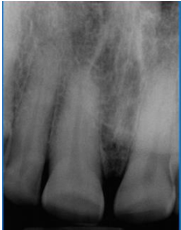
In comparison, this pre-operative radiographic image for tooth #4 shows more than 50% loss of tooth structure due to existing large restoration and decay.
Top crown denial code for inadequate criteria
The code associated with these types of denials is 5C4 (submitted documentation doesn’t support payment for full crown coverage).
Is structural damage caused by factors other than wear and abrasion?
Full crowns placed to repair lesions due to wear, attrition, abrasion, erosion or abfraction aren’t covered under most plans. A tooth must show a significant structural loss from decay, large restorations or fracture not attributable to the aforementioned causes.
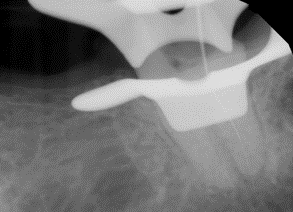
In the following example, the claim was submitted for crowns on teeth #8 and #9. However, pre-operative radiographic images show incisal wear. Restorative procedures to repair lesions due to wear, attrition, abrasion, erosion and abfraction aren’t typically covered.
Top crown denial code related to wear and abrasion
The code associated with crown denials due to the presence of wear, attrition, abrasion, erosion and abfraction is 510 (documentation does not support payment for full crown coverage, as the services will restore tooth structure lost due to wear, attrition, abrasion or erosion).
Does periodontal health support the use of a crown?
You must consider the periodontal health of a tooth before placing a crown. Teeth with uncontrolled or untreated periodontal disease typically don’t have a good long-term prognosis and won’t be considered for full crown coverage. For teeth with periodontal involvement, you’ll need to provide documentation of the current periodontal status and history of definitive treatment.
This example is from a claim for a crown on tooth #20. The claim was denied because pre-operative radiographic image depicts excessive bone loss.
Top crown denial code related to periodontal disease
The code most often associated with crown denials due to uncontrolled or untreated periodontal disease is 5A2 (submitted documentation shows that the long-term prognosis of the tooth is questionable due to excessive loss of bone support).
Has any endodontic disease in the tooth been appropriately treated?
You need to consider the status of an endodontically treated tooth. Don’t place a full crown on a tooth with untreated or unresolved periapical or periradicular pathosis. You must submit pre- and post-operative periapical radiographs for endodontically treated teeth.
The following radiograph was submitted with a claim for a crown on tooth #13. Because the pre-operative radiographic image shows untreated periapical pathosis, the claim was denied.

In this next example, the pre-operative radiographic image, submitted a claim for a crown on tooth #19, shows unresolved periapical and periradicular pathosis.

This example is for a crown on tooth #13, but the pre-operative radiographic image shows a poor or short fill of the existing root canal. The material used to fill the root canal does not seal the root.
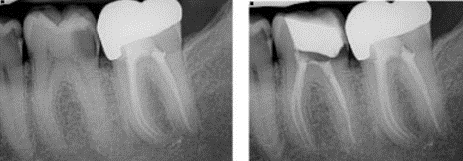
The following example was submitted with a claim for a crown on tooth #18. However, the pre-operative radiographic image was taken to measure the working length and doesn’t show the completed root canal. This x-ray may be submitted as a pre-operative x-ray, but it doesn’t qualify as a final endodontic film.
In comparison, the following radiographic images correctly depict an acceptable pre-operative periapical x-ray and post-operative x-ray of completed root canal therapy on tooth #19.
Top crown denial codes related to unresolved endodontic disease
The codes most often associated with crown denials due to untreated or unresolved periapical or periradicular pathosis and poorly filled root canals are:
- 5C2. The long-term prognosis of the tooth is questionable due to unresolved periapical or periradicular pathology.
- 5B3. The long-term prognosis of the tooth is questionable due to unresolved periapical or periradicular pathology of the existing root canal.
- 5E3. The long-term prognosis of the tooth is questionable because the placement, density or depth of the existing root canal filling material doesn’t provide an adequate seal.
- FMW. We couldn’t determine benefits because of missing pre- and post-operative periapical images.
- 8L9 and 586. We couldn’t determine benefits because of missing post-operative radiographic images of root canal therapy.
Best practices for crowns
To speed up processing and to make sure we can determine coverage for crowns, always review associated criteria and submit mounted and dated x-rays or supporting documentation.
Please refer to the submission requirements table (pages 4-1 through 4-3 of the 2022 Claims Processing Policies and Procedures Handbook, available in the Dentist Handbook) to see what documentation and clinical information we need for specific procedure codes. You can also refer to the specific procedure code in the handbook for more details about the description of procedures.
Don’t submit original radiographic images if they are the only diagnostic record for your patient. You can submit duplicate radiographs or radiographic image copies of diagnostic quality, including paper copies of digitized images. We can’t return radiographic images or other documentation submitted with paper claims. However, we will make an exception if you send us a stamped, self-addressed envelope with the claim.
If you have a unique case, please provide a full description and any supporting documentation to help our staff determine benefits. During a clinical review of claims and pre-treatment estimates, Delta Dental can request radiographic images and documentation for procedures that may not initially need any documentation.
Stay tuned for more tips
These tips will help you get your claims approved and receive payments more quickly. But there’s more to discuss. Next month, you’ll learn the do’s and don’ts of submitting claims for build-ups, post and cores and temporary crowns.
CDT coding and nomenclature are the copyright and a trademark of the American Dental Association, all rights reserved.
Recent posts
- Parent-approved ways to help calm anxious pediatric patients
- Oral health care for seniors: Improving access, improving outcomes
- Simplify your credentialing with CAQH: Check out our webinar recordings
- Updated 2026 CDT codes are here
- View our CDT 2026 Updates webinar and stay on top of code changes
- EFT will become our standard payment method starting 1/1/27
- Start the year strong: Key reminders to support your practice in 2026
- Discover 3 tips to power up your practice with new workflows
- Updated 2026 CDT codes are here
- Partner with us to improve the health outcomes of our shared members
